What is Perimenopause?
Perimenopause is the period leading up to menopause. This marks the end of our reproductive ability and is the natural end to ovarian function and the end of your menstrual period. This process can be up to two to twelve years before your periods stop. Menopause begins one year after your last period.
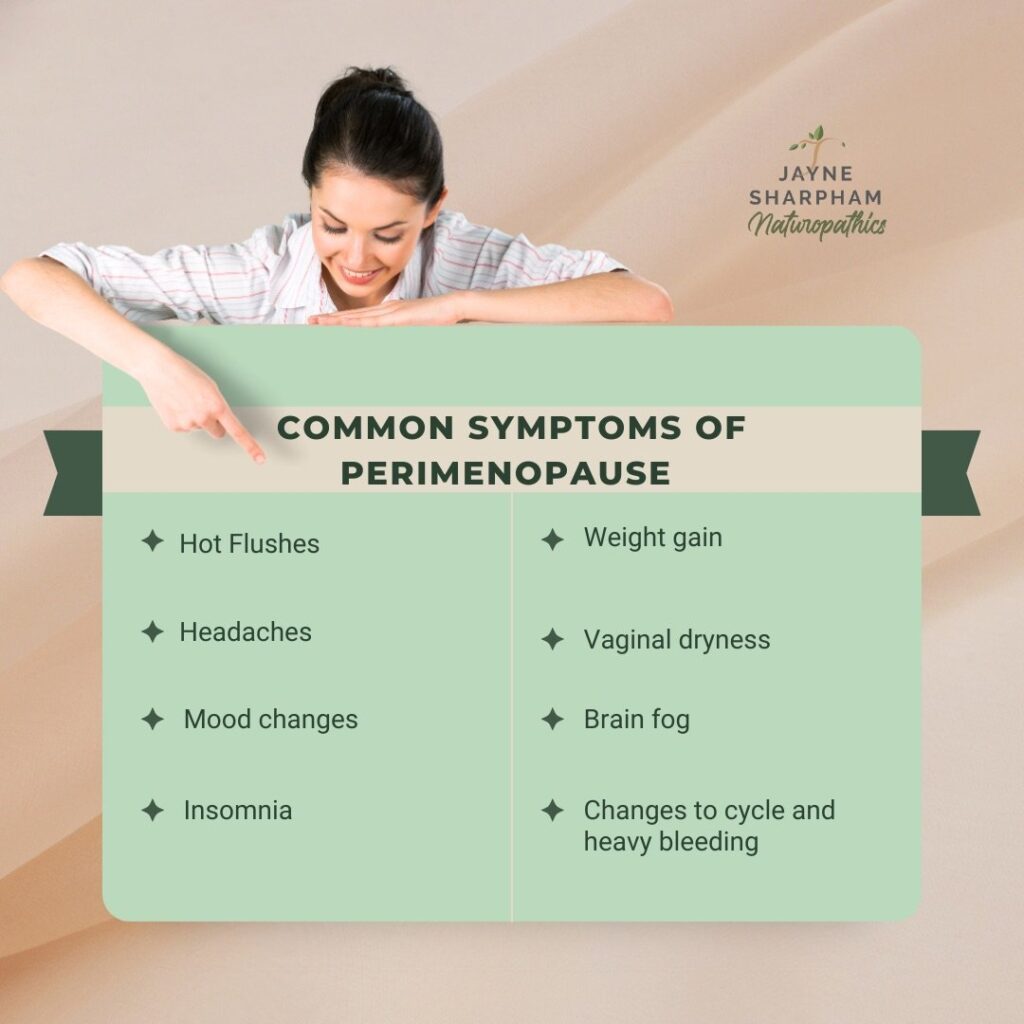
Perimenopause can be a turbulent time for some. You may be experiencing mood changes, irritability, depression, irregular cycles, breast pain. All of these symptoms can be triggered by hormone changes during this time. I will help guide you through the changes that may happen, so it is not something to be feared. Knowledge is power. This is a natural transition for you as a woman. Most of the symptoms you may be experiencing are temporary.
Perimenopause is a sequence of events for your hormones. Let’s unpack this so we understand what is going on.
Understanding our menstrual cycle
Firstly, we need to understand our menstrual cycle. Natural menstrual cycles are good for us as women.
The menstrual cycle is a natural process that typically lasts 28-32 days. It is controlled by reproductive hormones, mainly oestrogen and progesterone, involving a series of changes in the uterus and ovaries. It can be divided into four phases:
1. Menstrual bleeding. This is the first phase of the menstrual cycle, and it is classified as day 1. During this phase, the uterus sheds its inner lining, resulting in the discharge of blood and uterine lining through the vagina.
2. Follicular phase. This phase begins after menstruation finishes and lasts about 14 days. During this phase, the body prepares for ovulation, which involves the growth of one of the follicles in the ovaries. As the follicle grows, it produces oestrogen, which stimulates the thickening of the uterus lining.
3. Ovulatory phase. This is typically midpoint of the menstrual cycle, generally around day 14. It is when a mature follicle of the ovary releases an egg via the fallopian tube. The egg can be fertilised by sperm, which leads to pregnancy.
4. Luteal phase. This phase occurs after ovulation and lasts around 14 days. The follicle that released the egg becomes the corpus luteum, which produces progesterone. Progesterone helps prepare the uterus for possible implantation of a fertilised egg. If fertilisation does not occur, the corpus luteum breaks down and the menstrual cycle starts again.

Each natural menstrual cycle, you make a large amount of oestrogen in the days prior to ovulation and then you have a larger surge of progesterone in the two weeks after ovulation.
We only have a set number of ovarian follicles as women. By our forties, the shifts of peri-menopause occur because of the natural failure of ovarian follicles. Some cycles will no longer produce an egg, known as an anovulatory cycle. This makes oestrogen but not progesterone. Sometimes, you may still ovulate but you will have a very short luteal phase (which is the second part of your cycle) and this results in a smaller amount of progesterone produced also.
This leads to losing progesterone. If you are losing progesterone, you can start to experience higher oestrogen. Sometimes this is up to three times higher! This oestrogen can then fluctuate through this time, creating a rollercoaster of hormones. This is what leads to symptoms of breast pain, anxiety, irritable mood, heavy periods. Perimenopausal hot flushes are triggered by a fluctuation of oestrogen during this time as well as the effects oestrogen has on mast cells and histamine.
Perimenopause will happen in phases, and each woman may experience these stages for different time periods.
– Very early peri-menopause- approximately 2-5 years with regular periods and slight changes to those cycles.
– Early peri-menopause is the onset of irregular cycles (mean age for this is 47.5years old)
– Late Menopause transition is the first cycle of more than sixty days
– Late perimenopause is the 12 months from the final period
Menopause is a life stage that begins 12 months after your final period. After your final period, you move into having lower oestrogen. This is a natural part of this life stage. This oestrogen can fluctuate during this time and this can lead to menopausal symptoms of hot flushes, insomnia, vaginal dryness and memory loss.
If you have had a forced menopause due to medical induction or surgery these phases will not occur, you will go straight into a very low oestrogen state. You may find your symptoms are stronger because of this. If you have had a hysterectomy but still have your ovaries, you will still go through all these phases but have hidden cycling. This can be a confusing time as there is no bleed to clue to what your cycle is doing. If this is you, its really important your hormones are tested appropriately so as you are not being treated incorrectly.
Follicle Stimulating Hormone (FSH) testing is sometimes used as a marker for menopause. Before peri-menopause it will be low. During peri-menopause it will fluctuate and therefore is not an ideal test during this stage as a diagnostic for menopause as it will swing from low to high. At menopause (12 months from final period) FSH will be high on a blood test.
At the new low oestrogen and progesterone stage of menopause there is increased risk of insulin resistance, diabetes and osteoporosis. We will talk about this more later. For now, let’s understand more about the most important hormone players in this life stage.

Oestrogen
There are several types of oestrogen.
Estradiol is the strongest and most potent oestrogen. It is made as part of the leadup to ovulation. Estrone is another type of oestrogen and we make this via our fat tissue. There are a few oestrogen metabolites in the gut also.
Estradiol is important for heart health, muscle mass, bone mass, brain health, metabolic rate.
Estrogen is the hormone that stimulates breast tissue and thickens the uterine lining. This is the hormone that is responsible for heavy periods, which can be an increased issue for peri-menopause women due to the increased levels produced. Progesterone is the “sister hormone” to oestrogen. They need to be in the right ratio with each other. As progesterone drops in peri-menopause in ratio to high oestrogen this can further compound issues.
Progesterone
Progesterone is a hormone that we all want lots of! We make progesterone from our adrenal glands, kidneys, as well as from the corpus luteum- a product of ovulation. Natural ovulation cycles are our best friend when it comes to hormone balance.
Progesterone is a beautiful hormone we all want for as long as possible. It is responsible for thinning the uterine lining, reducing heavy periods. It is a naturally calming hormone and is important for sleep. It is also important for our heart, muscles and healthy breast tissue.
For the first half of the menstrual cycle, estrogen is the dominant hormone, laying down the lining of the uterus. After ovulation takes place around day 14 of the cycle, progesterone is designed to be the dominant hormone. However, with the changes to ovulation that peri-menopause brings the balance between estrogen and progesterone is affected. When this happens, estrogen tends to dominate in the days leading up to our periods which can affect how we feel and function.
Its important to note that being on the contraceptive pill, IUD or hormone replacement is not giving natural progesterone. These drugs give progestin, which is similar to progesterone. It gives some of the same effects e.g. thinning of the uterus lining but it can also have some opposite effects including anxiety, hair loss, weight gain, high blood pressure. Progestin’s can act more like testosterone.
Other Hormones
There are other female hormones that can affect women going through peri-menopause such as androgens DHEA and testosterone. Regulator hormones such as thyroid, cortisol, SHBG, FSH, LH and prolactin may also may a role. We will discuss in more detail later about the role of DHEA, cortisol and stress.
Good news is there is so much we can do to support you through perimenopause!






Responses